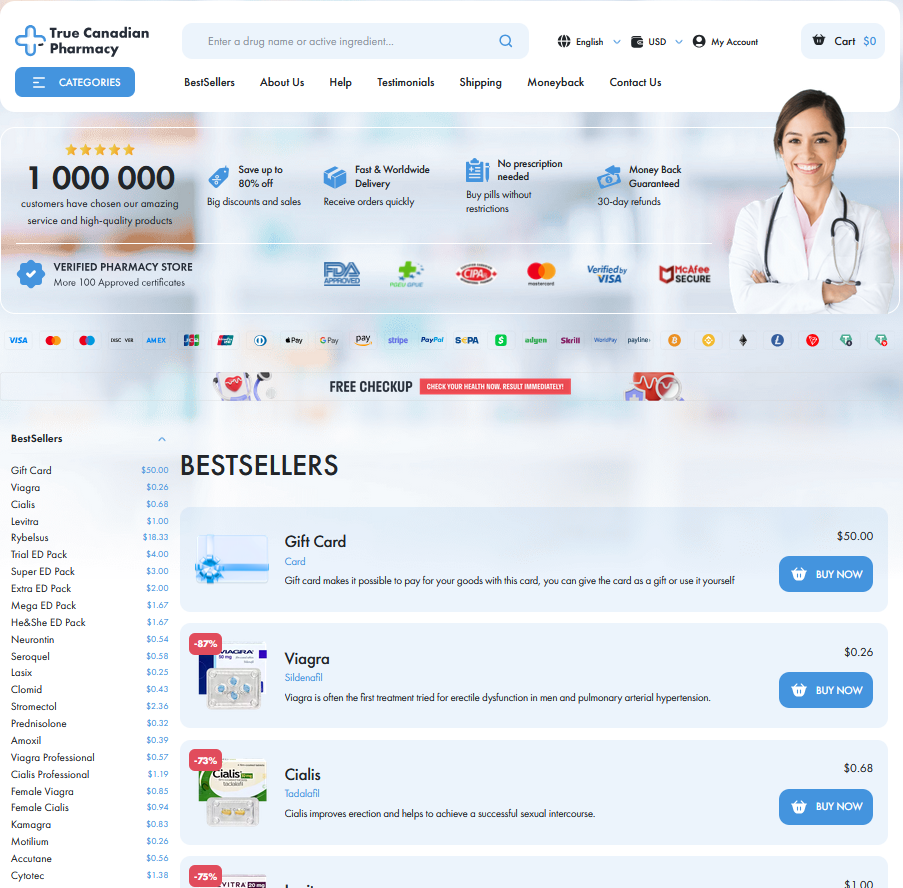
To Visit Online Pharmacy Click HERE ↓
Recognizing When Ventolin Isn't Enough: Next Steps
Signs Your Rescue Inhaler Isn't Providing Relief
I remember leaning against the kitchen counter, inhaler in hand, watching the clock as each breath stayed tight. When a quick puff doesn't ease wheeze, chest tightness persists, voice gets hoarse or you feel lightheaded, that's a clear sign the usual rescue dose may be failing. Cough that worsens despite use, or need to take the inhaler more than twice an hour, should raise concern.
Keep a log of episodes, noting triggers, time to relief and technique, and contact your clinician if relief is poor or use increases. They can reassess inhaler technique, consider stepping up controller therapy, and update an action plan with emergency instructions. Definately treat persistent poor response as a red flag.
When to Seek Emergency Care for Breathing

I remember the day my neighbor's wheeze wouldn't ease with a few puffs of ventolin; panic sharpened breath. When rescue inhalers stop working, watch for rapidly worsening shortness of breath, inability to speak full sentences, bluish lips or fingers, confusion.
If symptoms persist after repeated puffs, or your peak flow falls dramatically, don't hesitate: emergency evaluation can mean oxygen, nebulized bronchodilators, or steroids that stabilise breathing. Keep rescue inhaler technique correct and have someone call emergency services if you feel lightheaded, faint, or are gasping.
Document times and doses to help clinicians, and remember that symptoms can escalate fast; occassionally what seems mild can become life-threatening within minutes, so trust instincts and seek urgent care.
Track Inhaler Use and Symptom Patterns Closely
I started keeping a simple log after a sudden flare; noting time, trigger, and ventolin puffs gave immediate insight into patterns.
Record symptom severity on a scale and note activity, sleep quality, and medication timing; these data clarify when rescue therapy stops working consistently.
Share logs with your clinician; a pattern of frequent ventolin use or nocturnal symptoms may prompt treatment escalation or testing and written examples.
Small habits help: carry a pen, set phone reminders, and review entries monthly so you can act before attacks become severe Occassionally too.
Understanding Controller Medications and Stepping up Therapy

I remember coughing through a midnight storm reaching for ventolin that barely opened my chest. That moment taught me to look beyond quick fixes and learn why daily medicines exist to prevent those urgent scares.
Controller inhalers like inhaled corticosteroids long acting bronchodilators or combination inhalers calm airway inflammation and reduce flare frequency. Knowing each class and how they work helps you and your clinician craft a safer reliable regimen.
If symptoms persist clinicians step up therapy increase inhaled steroid dose add a LABA or consider biologics for severe allergic eosinophilic disease. Check inhaler technique adherence and triggers first small fixes often yield big gains.
Follow up visits peak flow and an updated action plan keep progress visible. Don't wait untill an ER visit collaborate on goals ask about side effects and carry both rescue and controller inhalers as recommended.
Reducing Triggers and Practical Nonpharmacologic Strategies
I remember the night my chest tightened despite using ventolin; panic mixed with a stubborn refusal to accept more meds. Start by scanning your home: stale air, strong fragrances, mould and pet dander often start attacks. Small changes can shift control.
Practical steps include improving ventilation, using HEPA filters, washing bedding hot, avoiding smoke and scented products, and keeping humidity low. Consider air purifiers and routine cleaning to reduce allergen load; these measures mean fewer rescues with ventolin.
Occassionally use masks during chores, and plan ahead for triggers. Track patterns and share notes with your clinician for smarter nonpharm strategies.
| Trigger | Action |
|---|---|
| Dust mites | Encased bedding wash weekly |
| Smoke | Avoid indoors ventilate windows regularly daily |
Collaborate with Your Healthcare Team for Action Plan
Begin conversations with stories: describe recent attacks, what helped, and when the rescue inhaler failed. Clinicians can map patterns and suggest measurable goals, making the problem feel less vague. Definately.
Ask for a written action plan outlining daily controller use, step-up steps for worsening symptoms, and exact thresholds for emergency care. Request inhaler technique review and peak-flow targets.
Schedule follow-ups to adjust therapy, and keep a symptom diary to share at visits; this partnership reduces surprises and helps you and your team respond quickly soon. NHS info American Lung Association



Pharmacy Hours
Mon - Fri: 09:00 am - 5:00 pm
Sat-Sun: CLOSED
After hours give us a call and we will arrange delivery for you.